We activated incident command immediately, and on Saturday began identifying and tracking all exposed employees, implementing airborne PPE, expanding testing, and implementing a communications network. We then experienced constant change.

For Aileen Mickey, MD, FCCP, chief medical officer and pulmonologist, EvergreenHealth Medical Group, Kirkland, Wash., a key challenge in managing response to one of the initial outbreaks of the novel coronavirus in the U.S. was navigating constant change.
EvergreenHealth includes a 320-bed regional hospital, a rural hospital, Evergreen Medical Group—including 48 clinics and 300 physicians and providers—and a large home health and hospice division. On Feb 27, the CDC expanded Covid-19 testing guidelines to include severely ill patients with lower respiratory infections without other explanations. Evergreen’s medical director of infectious disease decided to test two such patients in the ICU as a precautionary measure. Both tested positive.
“We activated incident command immediately, and on Saturday began identifying and tracking all exposed employees, implementing airborne PPE, expanding testing, and implementing a communications network,” said Aileen Mickey, MD, FCCP, chief medical officer and pulmonologist, EvergreenHealth Medical Group. “We then experienced constant change.”
As the CMO of a health care facility at the bleeding edge of the crisis, Dr. Mickey identified change as both hallmark and challenge in navigating a highly fluid situation in which guidelines from government agencies conflicted and changed rapidly as knowledge was acquired. As a result, guidelines for PPE level and conservation, testing protocols for patients and staff, policy for non-essential care, and return-to work-protocol for sick employees had to change on the fly, making communication one of the most important responsibilities of leadership.
PPE level and conservation. Initially, Evergreen instituted airborne PPE (PAPR and CAPR or N95 & Goggles) for every patient with or suspected to have Covid-19. But that swiftly changed as the State Department of Health recommended modified droplet and contact precautions for patients with Covid-19. Evergreen as well as the University of Washington moved to gowns, gloves, surgical masks, and goggles for patients who weren’t undergoing aerosolized-generating procedures (AGPs), such as nebulizers, intubation, or suctioning, which aerosolize droplets that cause infection. PAPR and CAPR and/or N95 and Goggles were reserved for patients undergoing AGP procedures.
In the ambulatory setting, any patient with respiratory symptoms and physicians and staff caring for them were masked, and EvergreeHealth eliminated all AGPs in clinic, such as nebulizers and including nasopharyngeal swabs for testing (which causes coughing if done properly).
PPE conservation tactics included:
Management of Exposed Employees. “The initial priority was to identify employees who had been exposed to the patients who tested positive, and we did this by going into our EMR and identifying anyone who had logged into the chart, and also self-reporting, because we have workers who may have gone into a room but didn’t log into the chart, such as Environmental Services,” Dr. Mickey explained.
The CDC recommended 14-day quarantine for any health care worker who came in contact with a patient infected with Covid-19, whether or not the worker had symptoms. “However, with the CDC in-house on Day 3 of this crisis, we quickly realized we could not staff the facility if we followed those guidelines,” Dr. Mickey said.
Therefore, Evergreen moved to active monitoring strategy to allow exposed asymptomatic employees to return to work. Employees undergo temperature checks twice a day, initially for exposed employees, but now for all employees. EvergreenHealth also started screening employees with symptoms to see if they met testing criteria and did this through a nurse call-in line (vendor: Healthline) and a text-based service (vendor: 98point6), where people could text in symptoms and they were run through an algorithm using artificial intelligence and a physician.
“We also quickly started work on an employee database to track exposed employees and test results,” Dr. Mickey shared.
Testing criteria. This was developed and changed multiple times, based on symptoms, risk factors, and special population characteristics. (See Figure)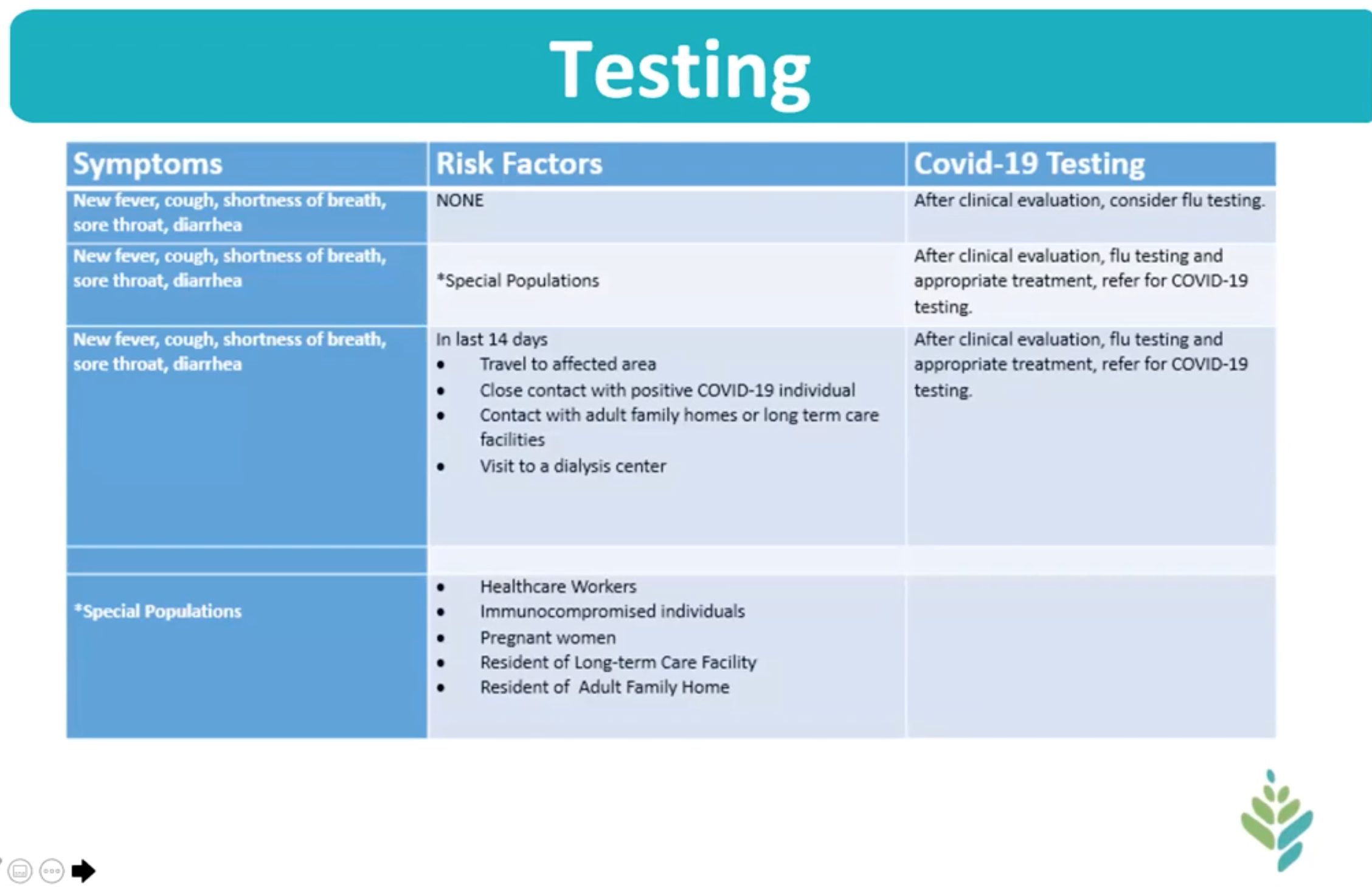
As of March 26, patients were triaged and tested according to the following protocols:
Visitation Policy. EvergreenHealth quickly limited patient visitors, and tightened that even further (see Figure):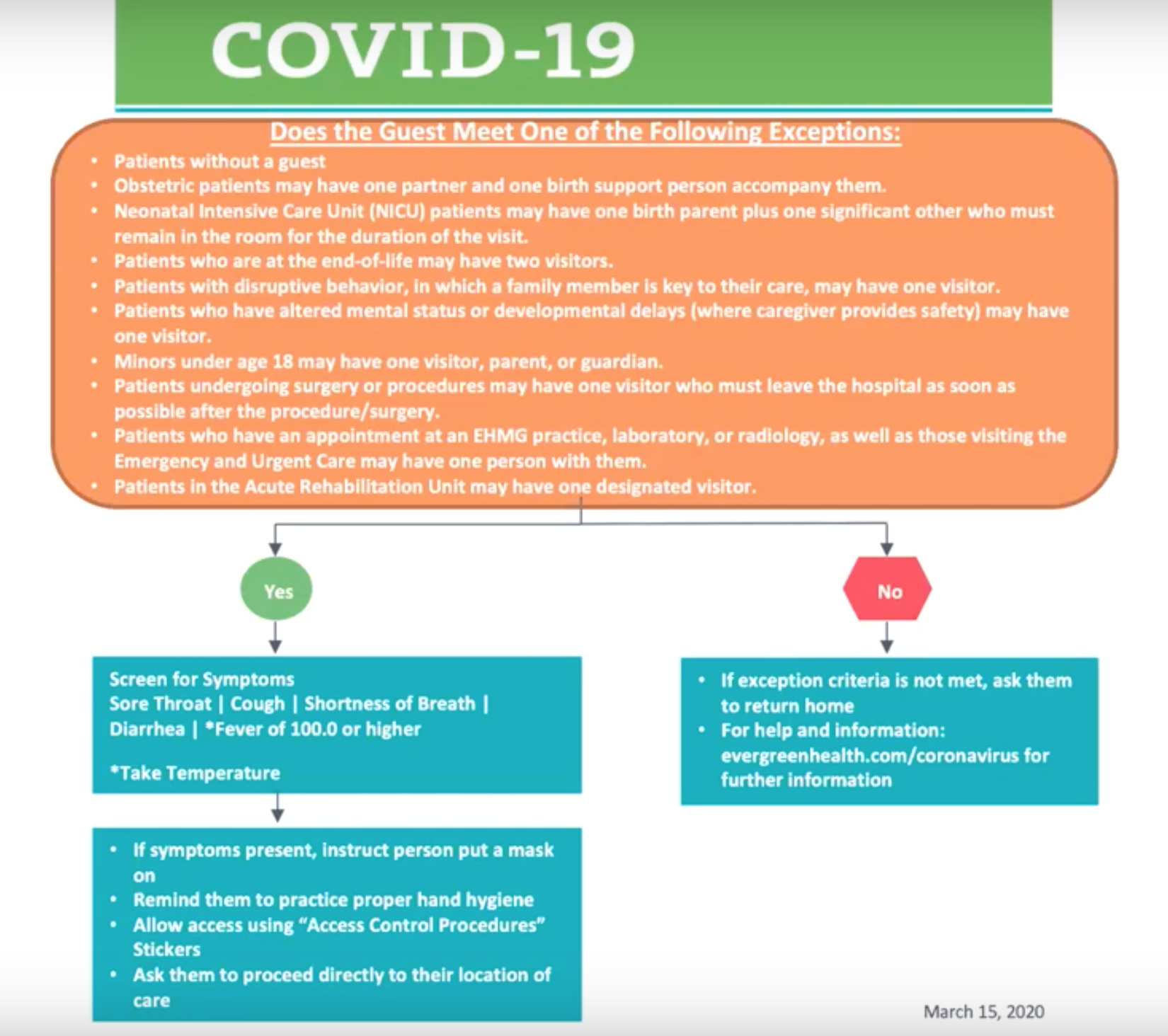
“Visitors and patients are screened as they come into the clinics and hospital entrances, and we are really trying to cohort sick patients,” she said.
Employee Monitoring and Return to Work. Dr Mickey described this as an ongoing work-in-progress.
Elective Surgery Policy. This policy also has evolved over time. A multidisciplinary task force set up when the first two patients were diagnosed met and determined that to keep patients safe and conserve PPE, certain surgeries need to be limited. Then the CDC in Kings County made the recommendation that all elective surgeries be cancelled. On March 13:
Non-essential Ambulatory Visits. CDC published recommendations for Kings County asking for limits on non-essential in-person visits. EvergreenHealth divided them into patients scheduled in the short-term, mid-term, long-term and developed the following strategies:
Short-term (0-2 weeks)
Mid-term (3-12 weeks)
Long term (> 12 weeks)
“We hope to re-establish services and procedures and maintain the short-term gains for the long term,” Dr. Mickey noted. “We are doing a lot very quickly in moving forward with telemedicine, such as video visits, and we want to preserve that work for the future.”
Care Venues
Communication
Communication was a key strategy of leadership from the start of the crisis. “You can never over-communicate in this situation,” Dr. Mickey emphasized. “Everyone is fearful including our employees, the patients, the community."
Internal communication included rounding, email, Web-Ex Town Halls, and daily leadership calls. External communication was executed by providing media access to interviews, sending email, notifications on the patient portal and web site.
Clinical Experience: JAMA
That communication also extended to the medical community, beginning with a review of EvergreenHealth’s first 21 cases written by a team of physicians from EvergreenHealth, the University of Washington, and the radiology practice Radia, and recently published in the Journal of the American Medical Association. Dr. Mickey shared the following data points:
"We currently have a database in process with a retrospective analysis of our data, we got IRB approval for that this morning, and we are in midst of chart review now hoping to get more data out to other health care organizations," she said. "We are participating in an antiviral study with the NIH, and we actually have the most patients in the country enrolled with 17, and our cap was just raised from 20 to 30, and may increase it as high as 50."
As of 3/26, EvergreenHealth tested 1,158 patients; 211 patients tested positive with 42 deaths.
Lessons Learned
Communicate continuously. “I can’t stress that enough,” Dr. Mickey said. “There is a lot of fear, things are constantly changing, there is a lack of continuity in messages being put out by DOH, CDC, other health care organizations, and it varies state by state. It gets incredibly confusing not only for patients in the community but for our health care workers.
Front-line input is imperative. “Our boots on the ground are dealing with patients, learning lessons,” she said. “They understand operations we have to get their input and change quickly and be flexible and nimble.”
Preserve PPE. “We want to keep our health care workers safe, but we also need to conserve PPE and use it appropriately,” she urged.
Plan for Surge. EvergreenHealth established a surge planning committee and converted beds over to negative air flow throughout their main hospital. “We’ve identified eight sites where we can put patients that don’t currently hold patients,” she added.
Implement telehealth. Video visits are a key tool.
Maintain Strict Testing Criteria. “With limited testing resources, it’s important to develop testing criteria and stick to them,” advised Dr. Mickey. “In an ideal world, we would test everyone to get the epidemiological data, but currently there is not a clinical reason to test people with mild disease.
She concluded by thanking the EvergreenHealth team and advising all to shelter in place: “As our Governor has said, we want to keep people at home: 'Stay home, and stay healthy'.”
Hub is the monthly newsletter published for the membership of Strategic Radiology practices. It includes coalition and practice news as well as news and commentary of interest to radiology professionals.
If you want to know more about Strategic Radiology, you are invited to subscribe to our monthly newsletter. Your email will not be shared.