Changes in how we get paid as a radiologist could be just as much of a disruption and just as much of an opportunity as AI. It just requires us to change the way we think about what we do.
Strategic Radiology's 33 independent practices decamped to Charlotte for the spring Membership meeting, including 12.5 CME credits and talks that included AI in practice, transitioning to peer learning, and a witty and informed state of the union address. Here's a recap.
Lisa Mead, RN, CPHQ, executive director of the Strategic Radiology Patient Safety Organization (SR-PSO), opened day one of the Quality Forum with a discussion of the top issues surrounding quality and patient safety. Staffing shortages sat atop the list Ms. Mead shared from ECRI's Leading Patient Safety Issues in Healthcare for 2022. “There are 1,400 job postings for radiologists, and we have 1,000 coming out of training,” noted Ms. Mead, adding that staffing shortages are being felt at every level of the radiology practice.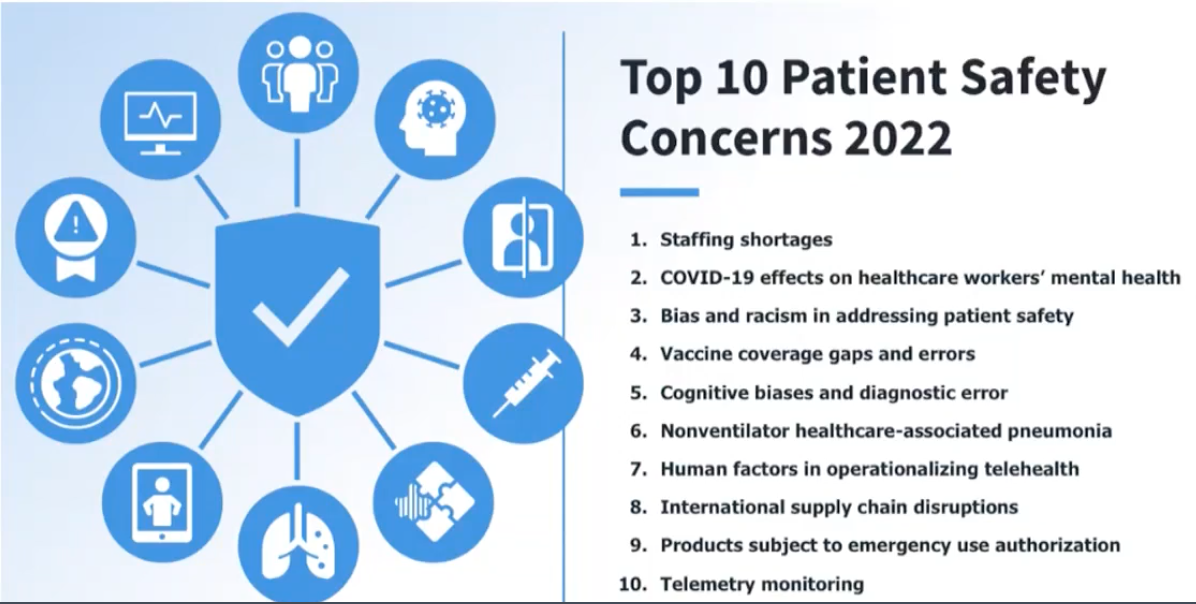
Sharing data from the medical malpractice carrier Coverys, Ms. Mead noted that claims rates and average-indemnity-paid 10-year trends are down, but radiology continues to be number 3 on the list of top specialties with multiple claims (defined as more than one claim in a ten-year period). “I know we are a bit protected because we are in a [malpractice] captive, but it is important to know that it continues to be a big issue, and radiology is not on the list of specialties getting a decrease in premiums.”
Diagnosis-related allegations are 23% of cases, surgery procedure related cases are number one at 27%, but surgery and diagnosis-related allegations are the costliest two categories and represent 57% of allegations and 59% of indemnity paid. “It follows that attention needs to be paid to this and that is why it is on our list of attention points in our quality strategy,” she said.
MIPS Value Pathways
CMS has teased a new, improved quality program for several years, and SR-PSO Medical Director Lauren Nicola, MD, president of member group Triad Radiology Associates, tag-teamed a session on the Merit-based Incentive Payment System (MIPS) Value Pathways, with Claudia Murray, MSN Healthcare, sr. VP of regulatory affairs and executive director of quality payment programming for MSN Healthcare.
‘I’m going to start by talking about something that has the potential to revolutionize the way we practice radiology, can differentiate those of us who participate and those who don’t, and can improve efficiency, quality, and outcomes. It can make us better or it can make us obsolete,” began Dr. Nicola. “How many of you think I’m talking about AI? Changes in how we get paid as a radiologist could be just as much of a disruption and just as much of an opportunity as AI. It just requires us to change the way we think about what we do.”
Dr. Nicola reminded that the MACRA legislation passed in 2015 created two pathways—APMs and MIPs. “MIPS were created as a pathway to APMs,” she explained. “We are going to focus on what CMS is doing to push all of us in the direction.” While CMS intended to move 50% of providers out of fee-for-service and into population-based payment models, the goal proved over-ambitious as many real-world obstacles arose, including meaningful ways to make physicians accountable for the cost of care. Another problem: how do you measure quality and put it on paper? “The idea of increasing the value of health care, improving quality while reducing cost is a great idea, but when you try to operationalize it, you hit a lot of speed bumps,” she said.
were created as a pathway to APMs,” she explained. “We are going to focus on what CMS is doing to push all of us in the direction.” While CMS intended to move 50% of providers out of fee-for-service and into population-based payment models, the goal proved over-ambitious as many real-world obstacles arose, including meaningful ways to make physicians accountable for the cost of care. Another problem: how do you measure quality and put it on paper? “The idea of increasing the value of health care, improving quality while reducing cost is a great idea, but when you try to operationalize it, you hit a lot of speed bumps,” she said.
Hence, the disillusionment with MIPS and the dawn of an intermediary program that CMS calls MIPS Value Pathways, which CMS will introduce for some specialties in 2023, participation voluntary. “Seven of the proposed pathways (Rheumatology, Stroke Care and Prevention, Heart Disease, Chronic Disease Management, Emergency Medicine, Lower Extremity Joint Repair, Anesthesiology) notice that radiology Is sort of peripherally involved, but none of them directly impact radiology,” she explained.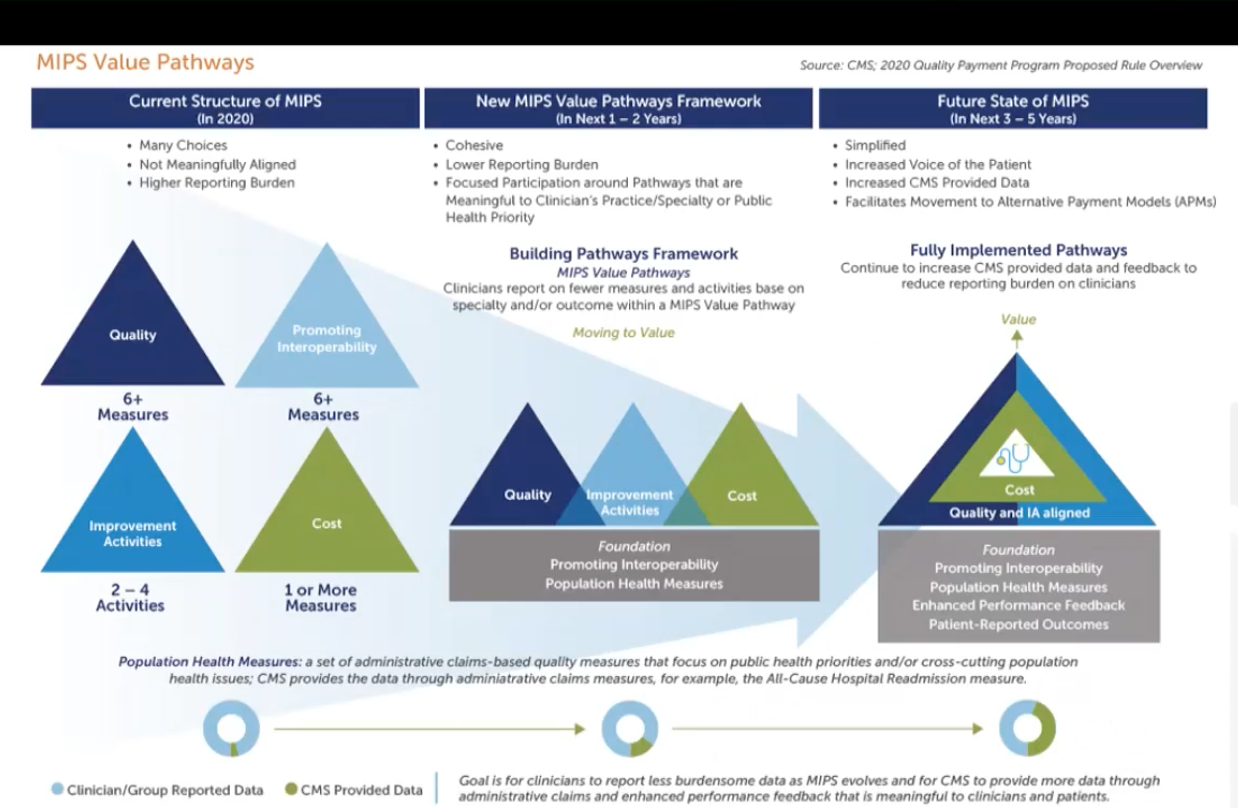
MIPS Value Pathways as conceived in 2020.
Ms. Murray took the microphone to lead SR through an MVP from another specialty, the Anesthesia MVP for 2023. MSN Healthcare provides billing and management services to both anesthesia and radiology and also operates a QCDR. “CMS proposed the Anesthesia MVP with the intent that it is for improving patient safety and support of a positive experience of patients with anesthesia,” Ms. Murray said. “The focus is on increasing quality of care, improving post-operative outcomes, promoting patient safety, enhancing satisfaction for patients receiving anesthesia.”
It essentially repackages existing quality measures, with some measures provided by the anesthesia society and a few cost measures associated with Medicare spend per beneficiary. Improvement activities also are bundled into the pathway, one of which centers on patient satisfaction, tying back to the measure.
Ms. Murray will follow this journey closely: As a QCDR, MSN must be ready to support its clients in 2023, and one anesthesia practice it services has agreed to test the MVP. “We are recommending to our anesthesia clients to build the mousetrap first,” she said, “So go ahead and play the game but plan to do the MIPS reporting as well. It’s going to be huge to do this at the group level, the subgroup level, and the registry level. We can do subgroups in 2023 but it is not mandatory. We are going to have to get this information from clients so there will be legal commitments and programming. That is major reengineering. What is supposed to be simpler is going to be more complicated to manage.”
The American Society of Anesthesiologists worked with CMS to be one of the MVP forerunners. “They wanted to stay in this game, and that is what I am proposing that we in radiology do too—do you want to stay in the game, or do you want CMS to propose that for you?” Ms. Murray queried.
“We certainly should not ignore this,” added Dr. Nicola, who is playing point on the MVP effort for the ACR. “MVPs may or may not be forced on us but we better be ready for them if they are.”
Dr. Nicola urged attendees to start thinking about how radiology can and does intersect with population health management. “Does radiology have a story?” she asked. “What about the breast cancer patient that doesn’t have to wait in the waiting room for hours because the technologist can get the radiologist to expedite a study. Can we do an incidental finding model? What about the studies that aren’t getting done? Educating referring physicians would be a great measure but the problem is tracking that. We have to be ready to tell our story.”
Scenarios from an Early AI Adopter
The coalition was privileged to hear twice from Ryan K. Lee, MD, MBA, radiology chair, Einstein Healthcare Network (now part of Jefferson Health), and an early adopter of AI; first on how to implement AI and secondly on how to leverage AI in peer learning programs. As an early adopter of AI, Dr. Lee shared practical lessons acquired as the market has quickly evolved.
He began by outlining the life cycle of a patient going through radiology—from ordering, scheduling, protocoling, acquiring, interpreting, reporting, reviewing, communicating the image. “Believe it or not, AI could touch all of these things.”
protocoling, acquiring, interpreting, reporting, reviewing, communicating the image. “Believe it or not, AI could touch all of these things.”
Scheduling. Although Dr. Lee’s department uses a scheduling software application, an actual human scheduler is still required to manually schedule radiologists for his department. “What if you had a scheduling software that uses AI, that knows how your practice runs—we have multiple specialists that cover multiple sites, and some specialists can cover more than one area. It gets very complicated very quickly, and I’m sure that some of your practices are even more complicated,” he said. “There are companies that can take that, learn how it can do it, and deploy radiologists in an intelligent manner. Take this a step further: what if you had 100 or 200 radiologists and multiple sites and you were able to predict, because you knew volumes based on time of year, holiday, weather, how deploy radiologists where they are needed? We are working with a company to do that right now.”
Reporting. Dr. Lee uses an algorithm that automates report impressions and believes it will categorically improve wellness among radiologists.
Communication. Closing the loop in communication is another area gaining traction in AI applications: “We partnered with a vendor to implement automatic patient notification for recommended studies,” he said. “We presented on this at RSNA and showed a modest 10% improvement in patients getting a recommended study.”
Peer Learning. One of the feedbacks Dr. Lee got from Einstein radiologists when they implemented peer learning was that it could be onerous. “There is a lot more work that goes into it,” noted Dr. Lee. “Can AI help with that, can it help in giving feedback to the radiologists?” Editor’s Note: We will share more about what Dr. Lee shared on that topic in a future issue.
Dr. Lee is using a plethora of diagnostic algorithms some of which are not FDA approved and require an IRB.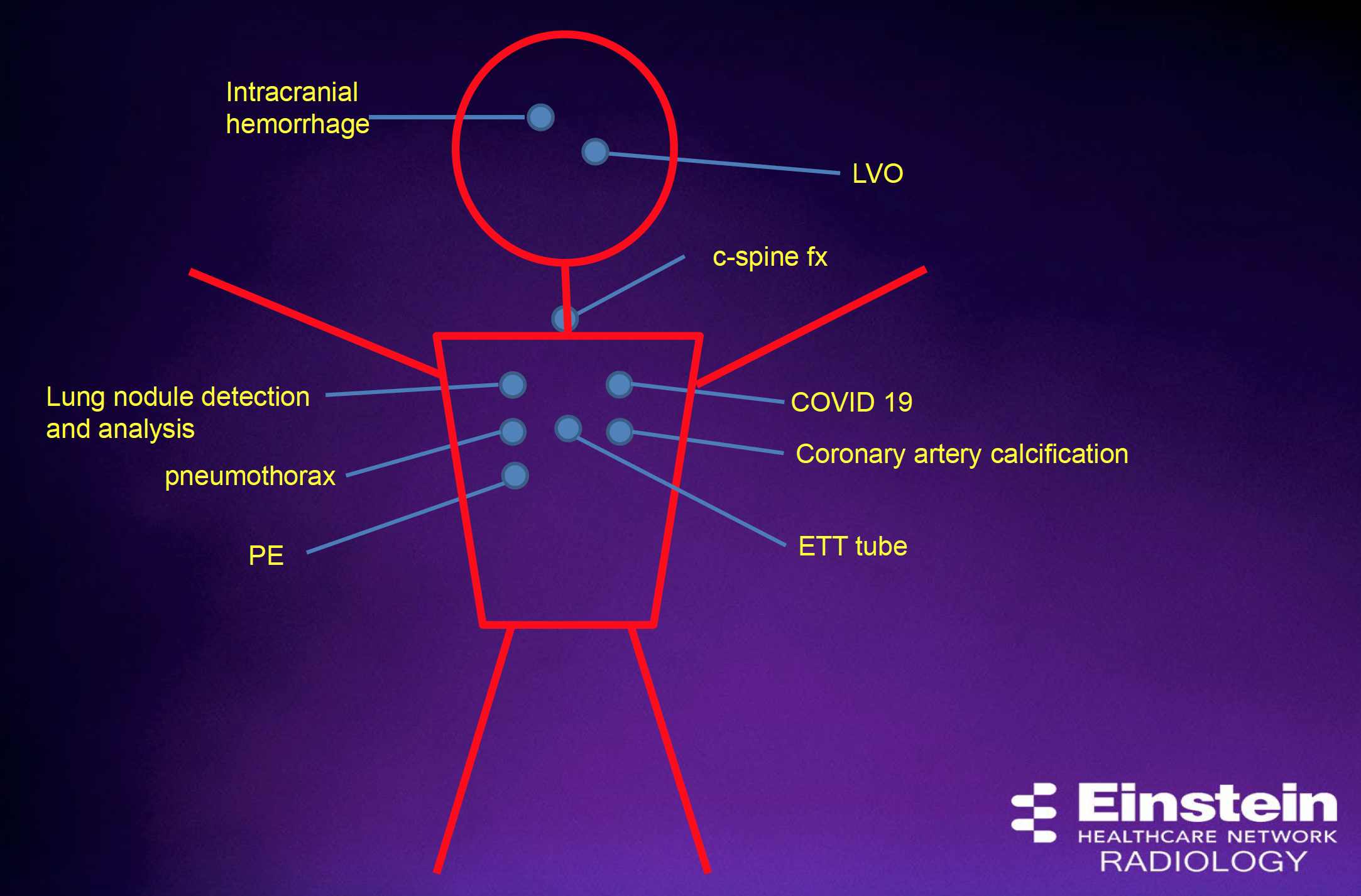 “They are not all great, in fact the vast majority are probably mediocre,” he said. “There are some that are excellent. Here’s the question: what do you do with all of them? Imagine having all of these on your workstation, how many screens would you need? Even if you have four screens, you have all of these different widgets deployed differently. That’s going to be an issue down the line.”
“They are not all great, in fact the vast majority are probably mediocre,” he said. “There are some that are excellent. Here’s the question: what do you do with all of them? Imagine having all of these on your workstation, how many screens would you need? Even if you have four screens, you have all of these different widgets deployed differently. That’s going to be an issue down the line.”
With so many AI applications for radiology in the marketplace and as more practices adopt these AI widgets, radiologists will have to be reminded to use them. “Ecosystems are the likely answer,” Lee said, referencing the iOS and Android ecosystems that have succeeded in encouraging developers to adopt their standards. In radiology, PACS and dictation systems are the obvious ecosystems, but some AI vendors are stepping forward to enter the fray (see related story on Ferrum Health).
AI has the potential to give radiologists a more prominent role in population health management, Dr. Lee asserts. “What if we could give the clinician, or the patient, information, incidentally, about their high -risk status, because they have high coronary calcification scores or they’re at risk of fracture due to osteoporosis?” he asked. “All of this information is already in the studies. All of these things can help all of us with what we have to do, but more importantly they can help the patient.” Dr. Lee acknowledged that the radiology department is working with cardiology and pulmonology at Einstein Healthcare Network to assist in development of a lung nodule and screening program.
All of this automation is welcome news to radiologists, but Dr. Lee emphasized that radiologists have a critical ethical role to play in ongoing monitoring or these algorithms to ensure that they continue to work as expected while ingesting datasets that are likely different than the training datasets. Another unsettled question is use of patient data: Should radiologists inform patients that an algorithm has been used in their care?
Be aware of the potential for bias, Dr. Lee added. “Watch out for bias, racial bias and radiologist bias in errors of commission,” Dr. Lee cautioned. “Is the algorithm taken as gospel, is the radiologist falling prey to these errors of automation bias?”
Practical Considerations
In conclusion, Dr. Lee offered these practical considerations in deploying AI:
1) Expense. You probably aren’t going to get paid for most of this. “Same as PACS and dictation systems, there is an expense to it and ultimately everyone will have to decide for themselves based on is it worth it from the financial POV and the patient and radiologist POV,” he said.
2) Vendors. Assess how good they are at supporting their product and be realistic about your practice IT capabilities and relationship with the hospital IT department.
3) Ongoing Monitoring. If inputs change over time, data drift can impact the performance of the algorithm. “You need a really good system to monitor these things and I don’t think they exist yet,” he said.
Dr. Lee again emphasized the radiologist role in deploying AI. “The ethical concepts we discussed are not AI concepts, they are human concepts,” he reminded. “We can treat AI as a tool to use, and that is what the Data Science Institute is designed for, to assess tools that help us take care of patients better. It is really not artificial intelligence, it is augmented intelligence, and in working with these tools, we can take better care of patients.”
The first day of an excellent meeting concluded with additional talks from:
Day Two: Multi-generational Workforces, State of the Union, the OBL Opportunity
The second day of the meeting got off to a lively start with a panel discussion billed as Managing Multigenerational Workforces featuring the president of member practice Mecklenburg Radiology, James Johnson, MD; Kurt Schoppe, MD, MBA, president-elect, member practice Radiology Associates of North Texas; and Jessica Montgomery, MBA, COO, member practice The Hill Medical Group, Pasadena, CA; and moderated by Ms. Mead and Barbara Perez Deppman, FACHE, FRBMA, SR COO. Ironically, the biggest takeaway was a warning against making generational assumptions and the suggestion that stage-of-life could be a more important predictor of behavior than generation.
Ford Koles Jr, health care economist with the Advisory Board, provided a witty and provocative overview of a health care environment that is highly unstable and extremely rip for change. Said Koles: “We built a system based on a reimbursement model that is fading. In any industry in which you have significant disequilibrium, you will have change. My point is which way do you want it to go? I think you can anchor your future in six inflection points: price transparency, value-based care, physician alignment, virtual care, home-based care, and health equity.”
In the ever-changing world of radiology reimbursement, there are occasions in which the stars align, and an entrepreneurial opportunity emerges. Some SR groups are recognizing that an could be both a route to greater IR well-being as well as a rare outpatient service line with profitability potential. Profitability, however, is not guaranteed. The cost to equip a state-of-the art OBL that enables the broadest IR service line options is quite high, and the endeavor requires hard work and sustained marketing.
The focus that afternoon was on an emerging entrepreneurial opportunity for outpatient interventional radiology, the outpatient-based lab (OBL). A terrific program was provided by Harry Curley, CEO of Streamline MD, and Phil Pease and interventional radiologist Gerald Niedzwiecki, MD, both of Endevir, who shared liberally on how to set up a lab, procedure caseloads, and success pearls and pitfalls. Ray Beauchamp, MD, Radiology Associates of Richmond, and JP DeVincenzo, Radiology Associates of North Texas shared on their experiences in this space.
If you haven’t already made plans to attend the fall Quality Forum, Leadership Development and Membership Meeting, September 16–18, in Dallas–Fort Worth, reserve your spot now.
Hub is the monthly newsletter published for the membership of Strategic Radiology practices. It includes coalition and practice news as well as news and commentary of interest to radiology professionals.
If you want to know more about Strategic Radiology, you are invited to subscribe to our monthly newsletter. Your email will not be shared.